The National Hospital Insurance Fund (NHIF) employees will undergo vetting before being absorbed into the Social Health Authority (SHA), with an aim of eliminating corrupt public individuals.
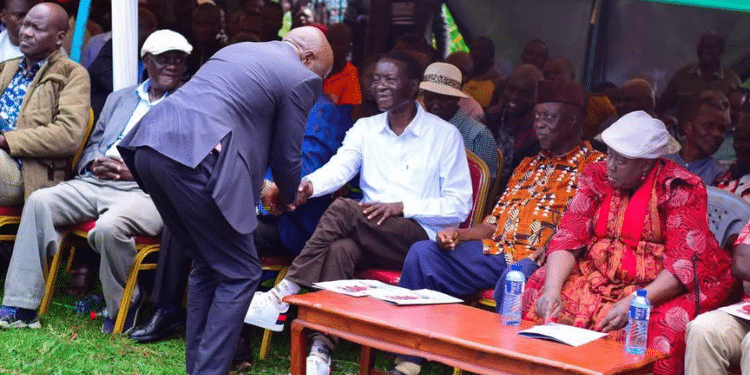
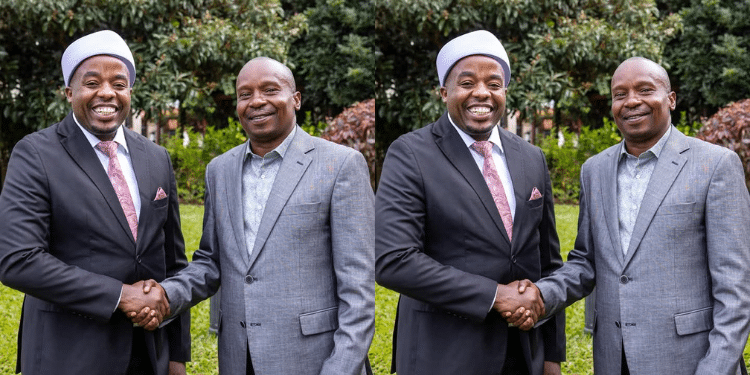
Speaking during the handover of NHIF graft report on Tuesday, March 5 by Ethics and Anti-Corruption Commission (EACC) to SHA, Principal Secretary for Medical Services, Harry Kimutai maintained that only staff who will pass the vetting process will be transitioned to the new authority.
“We want to make sure operations of social health authority that we are going to put in place are going to support and to ensure that there’s no more fraud in the claims a challenge that NHIF has faced for a long time,” Harry Kimai said.
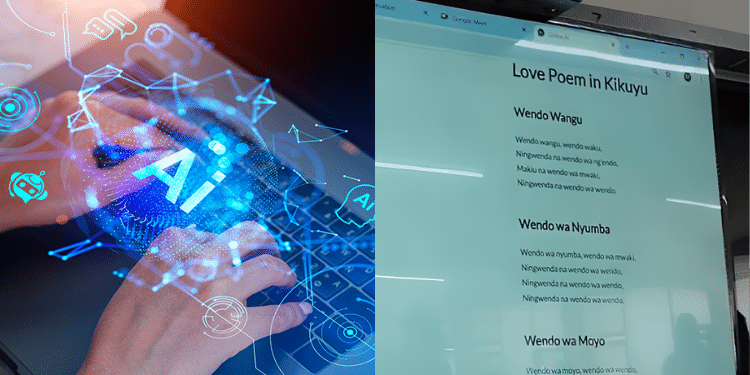
The anti-graft agency released the findings following an examination of systems, policies, procedures, and practices of work at the NHIF.
EACC found out that corrupt officials collaborated with healthcare providers to siphon funds from the organization.

The report was a result of the findings and recommendations from a recently completed examination into the systems, policies, procedures and practices of the defunct NHIF.
Also Read: Govt Reveals How NHIF Lost Ksh20 Billion to Hospitals Through Fraud
NHIF Employees Looting Public Funds
The report revealed that some three NHIF staff irregularly amended member details occasioning a loss of Ksh29.9 million to the fund on 14th July 2022.
In addition, 12 specialized Services were added to one health care provider and privileged transactions were carried out by unauthorized users in the e-claim system assignment.
The report also revealed that there was withdrawal of fast in fast out formula over right rights and adding and removing of service codes to health care providers facilities.
Other malpractices recorded included amendment to members and health care provider data and processing of transactions without approval workflows.
There was also failure to promptly migrate user system profiles for transferred staff and sharing of system access credentials between staff and interns.
Furthermore, the report highlighted delays and inefficiencies in the re-contracting process for healthcare providers, leading to operational challenges and potential losses for NHIF.
“The timelines for health care providers Contracting for various packages were not defined applications took 18, 20 and 50 months to receive approval for appointment to the fund panel of providers,” the report read.
Also Read: REVEALED: When Kenyans Will Stop Using NHIF Cover
EACC to take on Corrupt Individuals
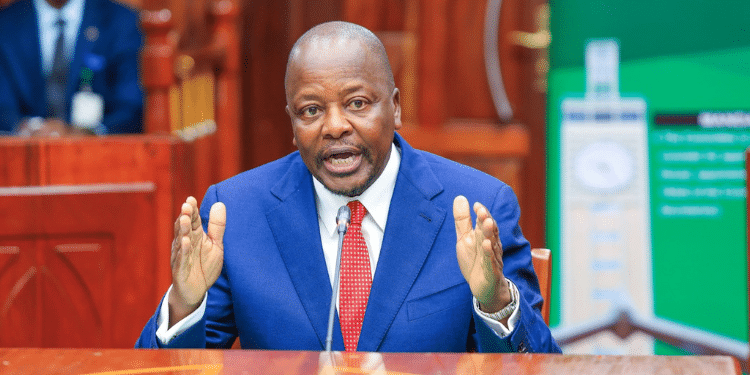
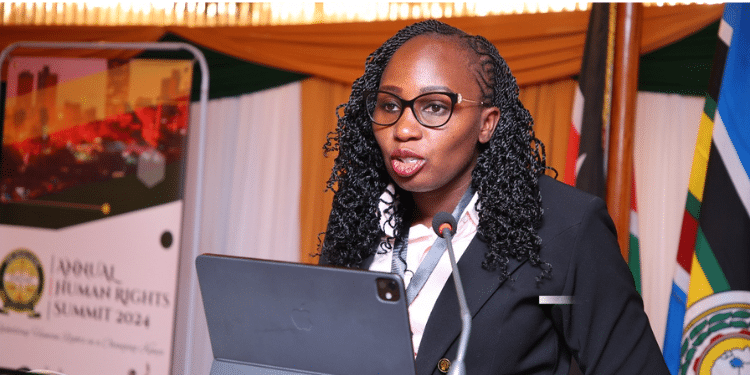
EACC chairperson David Oginde said that they will support the Board in sealing the identified corruption loopholes and systemic weaknesses even as investigations on the criminal aspects continue.
“Any resources that were stolen from or through the NHIF will be pursued until they are brought back or the people who were involved are brought to book.”
“Where individuals are found to have illegally benefitted from public funds, the Commission will, besides recommending prosecution, file civil suits to recover the lost funds,” he said.
Dr Oginde further said that the Commission expects the Management of the Social Health Authority to come up with an implementation plan for the Report within 30 days. The Commission will monitor the implementation process.
In his remarks, the SHA chairperson Timothy Olweny said that the report will guide governance reforms in social health insurance and ensure that the Social Health Authority will not have any loopholes witnessed in the report.
“We have to be able to enhance our fraud detection systems and fraud prevention systems and that’s why this report comes at a very opportune time for us because it helps us to be able to modify any systems that we were designing at this stage,” he said.