A survey conducted across 27 counties in Kenya, reveals a worrying trend regarding the prevalence of Obstetric Violence (OBV) experienced by women in Kenya.
The survey by Nguvu Collective centered on OBV experienced by women during pregnancy, childbirth, and the postpartum period.
Additionally, the study, which engaged 189 participants, shed light on the harrowing experiences faced by women, with 83% reporting at least one form of OBV.
The study, titled “Towards Ending OBV in Kenya -Unveiling the Invisible Wounds of Obstetric Violence Through the Voices of Kenyan Women” revealed various aspects surrounding OBV, pointing out its impact on maternal, infant, and child health, as well as the systemic factors contributing to underreporting.
Among the key findings is that OBV transcends geographical boundaries, with responses gathered from 27 counties across 7 provinces in Kenya.

Shockingly, 11% of the respondents identified as women with disabilities, pointing to the intersectionality of OBV with other forms of marginalization.
“83% of women who participated had experienced at least one form of OBV, 11% were women with disabilities,” reads part of the survey.
The survey also unveiled the socioeconomic disparity prevalent among survivors, with 51% hailing from low-income or below-the-poverty-line households.
Furthermore, a significant proportion of women affected by OBV fell within the age range of 25 to 34 years, comprising 46% of the respondents.
Forms and Occurrences of OBV
Psychological and emotional abuse emerged as the most prevalent form of OBV, affecting 62% of the respondents.
This included instances of verbal abuse, humiliation, and discrimination.
Physical violence and coercion were reported by 10% of the participants, with accounts of pressuring women into accepting unnecessary medical interventions or experiencing physical harm during pregnancy, childbirth, or the postpartum period.
Medical neglect, malpractice, and unnecessary interventions constituted 28% of OBV experiences, encompassing a range of violations such as denial of care, forced sterilizations, and non-consensual medical procedures.
Also Read: 1 in 3 Women Experience Sexual Violence by an Intimate Partner – WHO
Temporal Trends and Healthcare Settings
Likewise, the temporal analysis of OBV incidents revealed a concerning trend, with a notable surge reported between 2018 and 2021.
This period coincides closely with the onset of the COVID-19 pandemic, suggesting a correlation between healthcare disruptions, resource constraints, and increased incidents of OBV.
Notably, OBV was not confined to specific healthcare institutions, with incidents occurring across public hospitals (59%), private hospitals (16%), health centers (4%), maternity clinics (2%), and mission/faith-based hospitals (5%).
The involvement of multiple healthcare providers further shows the pervasive nature of OBV within the healthcare system, with nurses (51%), doctors/obstetricians/gynecologists (25%), and support/non-clinical staff (19%) identified as key perpetrators.
Impact on Maternal, Infant & Child Health
Similarly, repercussions of OBV extend beyond the immediate experiences of women, with 68% of incidents constituting gross human rights violations.
These violations, ranging from physical abuse to denial of care, not only deprive women of their fundamental rights but also have enduring consequences on maternal, infant, and child health.
Tragically, 9% of OBV incidents resulted in infant mortality, while 13% had long-term adverse effects on the health and development of the child.
Additionally, 13% of women reported physical injuries during childbirth due to OBV, showing the grave implications of mistreatment within maternal healthcare.
Underreporting and Barriers to Seeking Help
Despite the pervasive nature of OBV, 94% of women indicated that they did not report their experiences.
Fear of inaction (38%), retaliation (32%), and lack of awareness about reporting channels (35%) emerged as barriers to seeking help.
Moreover, feelings of stigma (17%) and normalization of OBV experiences (13%) further perpetuate the culture of silence surrounding this issue.
In response to these alarming findings, survivors emphasized the urgent need for parliamentary action to address OBV in Kenya, with 97% supporting formal legislative measures.
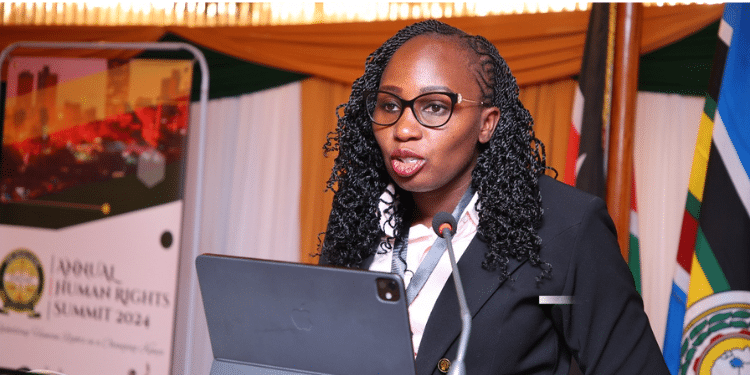
Ajra Mohamed, Partnerships Specialist at Nguvu Collective, voiced concerns about the gravity of obstetric violence (OBV), stating, “OBV is a shocking reality that has seldom been spoken about publicly.”
Also Read: Meet Six Women Leaders Challenging Gender Biases in Kenya
Mohamed pointed out the glaring issue of underreporting, highlighting that “94% of the women who participated in the survey said they did not report their OBV experience because they felt no action would be taken.”
Furthermore, the Nguvu Change Leaders, Harriet Afandi, Josephine Mwende, and Deborah Monari, stressed on the distressing accounts of abuse shared by women during the survey.
“The accounts of verbal, emotional, and physical abuse the women shared with us are deeply troubling and anguishing.”
“Every woman has the right to be treated with dignity. We cannot and should not ignore the stories that emerged through this survey. We plan to share the findings with key duty-bearers and request them to drive momentum in the Parliamentary debate on the need for a National Policy on OBV,” they said.